Immunotherapy has emerged as a groundbreaking treatment approach in the fight against cancer, harnessing the power of the immune system to target and destroy cancer cells.
Recent advancements in immunotherapy have led to the development of novel therapies that can effectively combat a variety of cancers, offering new hope to patients facing difficult diagnoses.
One major breakthrough in immunotherapy is the development of checkpoint inhibitors, which work by releasing the brakes on the immune system, allowing it to recognize and attack cancer cells more effectively. By targeting specific checkpoints that prevent immune cells from mounting an effective response, these inhibitors have shown promising results in improving patient outcomes and providing a much-needed alternative to traditional cancer treatments.
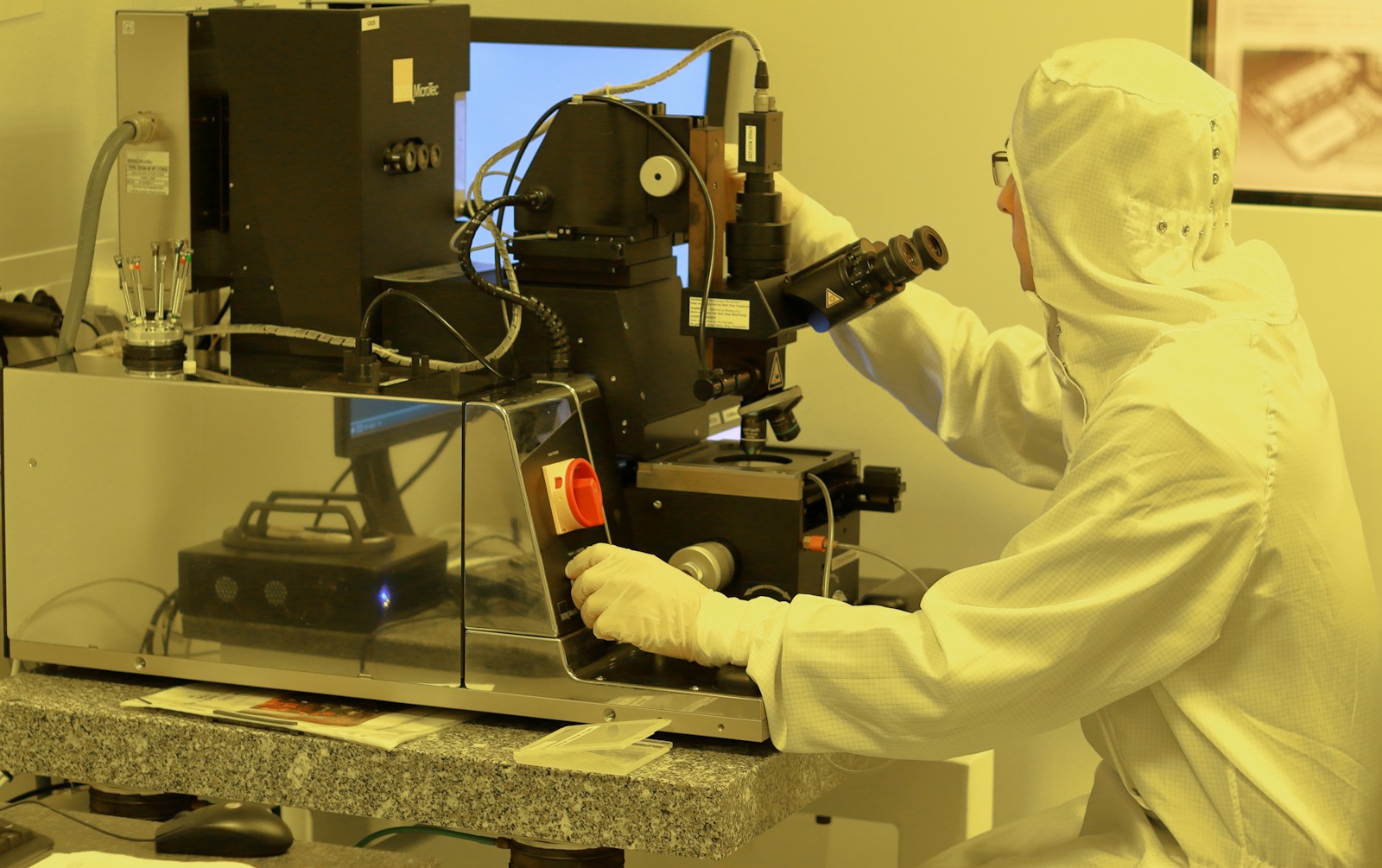
Genetic Engineering in Cancer Treatment
Advancements in genetic engineering have revolutionized cancer treatment, offering new possibilities for targeted therapies. By modifying genes, scientists are able to design treatments that specifically target cancer cells while sparing healthy tissue from damage. This precision allows for more effective and personalized treatment plans tailored to individual patients based on their genetic makeup.
One of the most promising applications of genetic engineering in cancer treatment is the development of genetically modified T-cells, also known as CAR-T cell therapy. This innovative approach involves modifying a patient’s own immune cells to better recognize and attack cancer cells. The results have been remarkable, with some patients experiencing complete remission of their cancer, showcasing the potential of genetic engineering to transform the landscape of cancer therapy.
Nanotechnology in Drug Delivery
Nanotechnology has revolutionized drug delivery by allowing for precise targeting of medications to specific cells or tissues in the body. Nanoparticles, which are particles on the nanoscale, can be loaded with drugs and designed to release them at the site of action. This targeted approach minimizes side effects and enhances the therapeutic effect of the drug. Additionally, nanoparticles can improve drug stability and solubility, increasing their bioavailability and effectiveness.
Another advantage of using nanotechnology in drug delivery is the ability to overcome biological barriers that may hinder the effectiveness of traditional medications. Nanoparticles can bypass the blood-brain barrier, for example, allowing drugs to reach the brain in the treatment of neurological disorders. Furthermore, nanotechnology enables the delivery of combination therapies in a single nanoparticle, maximizing the synergistic effects of multiple drugs. This customized approach has the potential to transform the field of medicine and improve patient outcomes significantly.
Artificial Intelligence in Healthcare
Artificial Intelligence in healthcare is revolutionizing the way medical professionals diagnose and treat patients. By utilizing AI algorithms to analyze vast amounts of data, healthcare providers can make more accurate and timely decisions, leading to improved patient outcomes. One of the key areas where AI is making a significant impact is in medical imaging, where it can assist in the early detection of diseases such as cancer through the interpretation of complex scans with greater precision.
Another important application of Artificial Intelligence in healthcare is in predictive analytics, where AI models can forecast potential health issues and recommend personalized treatment plans. By analyzing patient data, AI can help identify patterns and trends that may not be readily apparent to human healthcare providers, allowing for proactive interventions and preventative measures. As AI continues to advance, its integration into various aspects of healthcare holds the promise of delivering more efficient and effective patient care.
Stem Cell Therapy for Regenerative Medicine
Stem cell therapy has emerged as a promising avenue for regenerative medicine, offering the potential to repair and replace damaged tissues and organs. This innovative approach involves harnessing the unique properties of stem cells to stimulate the body’s natural healing processes and restore normal function. By directing the differentiation of these versatile cells into specific cell types, researchers aim to address a wide range of medical conditions, from degenerative diseases to traumatic injuries.
The versatility of stem cells, with their ability to self-renew and differentiate into various cell types, holds significant promise for revolutionizing the field of regenerative medicine. These cells have the capacity to regenerate damaged tissues, promote tissue repair, and support the body’s healing mechanisms. Through ongoing research and clinical trials, scientists are uncovering new applications for stem cell therapy that may ultimately transform the treatment landscape for patients with diverse health challenges.
Precision Medicine and Personalized Treatment
In the realm of healthcare, precision medicine is revolutionizing the way we approach treatment strategies for various diseases. By analyzing an individual’s genetic makeup, lifestyle factors, and environment, healthcare providers can tailor treatments to the specific needs of each patient. This personalized approach allows for more effective and efficient interventions, leading to improved patient outcomes and quality of care.
Moreover, the integration of precision medicine into clinical practice has the potential to drive advancements in early disease detection, targeted therapies, and preventative measures. By utilizing cutting-edge technologies and data analysis tools, healthcare professionals can better understand the underlying mechanisms of diseases and develop customized treatment plans that consider the unique characteristics of each patient. This shift towards personalized medicine is reshaping the healthcare landscape, offering new possibilities for more precise and individualized care.
Robotic Surgery and Minimally Invasive Procedures
Robotic surgery has revolutionized the field of minimally invasive procedures by providing surgeons with enhanced precision and control during operations. The use of robotic systems allows for smaller incisions, reduced blood loss, and faster recovery times for patients. With the assistance of robotic technology, surgeons can perform complex surgeries with greater accuracy, leading to improved outcomes and patient satisfaction.
The growth of robotic surgery has provided new opportunities for healthcare providers to offer advanced treatment options to their patients. As robotic systems continue to evolve and become more sophisticated, the potential benefits for patients are vast. From reduced post-operative pain to shorter hospital stays, robotic surgery is reshaping the landscape of modern healthcare by pushing the boundaries of what is possible in the operating room.
Brain-Computer Interfaces for Neurological Disorders
Brain-computer interfaces (BCIs) have emerged as a promising technology for individuals suffering from neurological disorders. By directly connecting the brain to external devices, BCIs enable patients to communicate and interact with the world around them, offering new hope for those with conditions such as amyotrophic lateral sclerosis (ALS) or spinal cord injuries. These interfaces bypass traditional neural pathways that may be damaged or impaired, providing a direct route for individuals to control devices or even prosthetic limbs using their thoughts.
Furthermore, BCIs have shown potential in helping patients with conditions like epilepsy or Parkinson’s disease by providing real-time monitoring and intervention. The ability to detect and respond to neural activity in such disorders offers a personalized approach to treatment, allowing for more targeted interventions and improved patient outcomes. As research in brain-computer interfaces continues to advance, the possibilities for enhancing the quality of life for individuals with neurological disorders are increasingly within reach.
3D Bioprinting for Organ Transplants
3D bioprinting, an innovative technology that allows for the creation of three-dimensional tissues and organs, is revolutionizing the field of organ transplants. This cutting-edge approach involves the layer-by-layer deposition of bio-ink containing living cells to construct functional tissues with complex structures. By mimicking the natural architecture of human organs, 3D bioprinting holds great promise in addressing the critical shortage of donor organs for transplantation.
One of the key advantages of 3D bioprinting is the ability to customize organs based on the specific needs of individual patients. This personalized approach not only enhances the compatibility between the transplanted organ and the recipient’s body but also reduces the risk of rejection. Furthermore, the precision and accuracy of 3D bioprinting enable the creation of organs with intricate vascular networks, which is crucial for ensuring proper blood supply and functionality post-transplantation. As research in this field progresses, the potential of 3D bioprinting to revolutionize organ transplantation and improve patient outcomes continues to expand.
Telemedicine and Remote Patient Monitoring
The increased use of telemedicine and remote patient monitoring has revolutionized the way healthcare services are delivered and received. Patients now have the convenience of consulting with healthcare providers from the comfort of their own homes without the need for in-person visits. This has proven to be particularly beneficial for individuals with mobility issues, those living in remote areas, and patients with chronic conditions who require regular monitoring and follow-up care.
Through telemedicine, healthcare professionals can remotely assess patient symptoms, provide medical advice, and even prescribe medication as needed. Remote patient monitoring devices allow for real-time tracking of vital signs and other health metrics, enabling healthcare providers to intervene promptly in case of any concerning developments. These technologies not only enhance patient convenience but also lead to better health outcomes by improving access to care and facilitating early detection and intervention of health issues.